- Clinical
- Laboratory
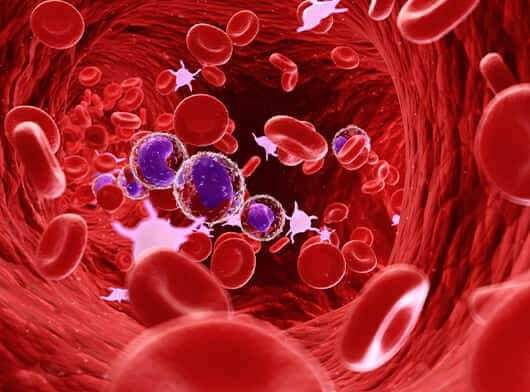
- Complete Blood Count (CBC) – to measure the amount of haemoglobin and the different kinds of red blood cells because people with Thalassemia have fewer healthy red blood cells and less haemoglobin than normal. This test includes MCV-mean corpuscular volume for to measure the red blood cells size. If the MCV is low and iron deficiency gets ruled out as a cause, Thalassemia should be considered.
- Haemoglobin(Hb) Electrophoresis – To know the types of haemoglobin problems, namely problems with the alpha/beta globin protein chains, such as Hb A, Hb 2A, Hb F, Hp S, Hb H, and so on.
- Iron profile – Includes serum iron, ferritin and total iron binding capacity (TIBC)To determine the amount of iron in the blood to determine whether the anaemia is due to iron deficiency or thalassemia.
- Blood Smear (called peripheral smear) – To know the number and types of WBC-white blood cells, RBC-red blood cells, and platelets - to see if they are normal and mature. With thalassemia, the RBC often appears smaller than normal.
- Family Genetic Study – Involves taking a family medical history and doing blood tests on family members to know whether the family members have missing or altered haemoglobin genes. This study can help determine the family member's risk of passing this disorder to their children.
- DNA Analysis or Molecular Test – To help confirm gene mutations. This is not routinely done but can be used to aid the diagnosis of Thalassemia if patients are already transfused and to determine carrier status if indicated. More than 250 mutations are associated with beta-thalassemia, such as HBB mutation. HBA1 and HBA 2 are the common mutations detected for alpha thalassemia.
- Prenatal Testing (Genetic Test)– It gets done when they are expecting a baby and other first degree family members (parents) are thalassemia carriers. This includes testing of the foetus during pregnancy at increased risk for thalassemia. This test is especially important if both parents carry a mutation because that increases the risk that their child may inherit a combination of abnormal genes and cause a more severe form of thalassemia.
- Blood Test - There are three important tumour markers for testicular cancer as
- Alpha-fetoprotein (AFP) - Any patient with an elevated AFP is likely to have a non-seminomatous component of testis cancer.
- Human chorionic gonadotropin (HCG) - The doctors can evaluate it in several other malignancies, including cancers of the liver, lung, pancreas, testicles and stomach
- Lactate dehydrogenase (LDH) is less specific for testicular cancer than HCG or AFP. However, elevated LDH levels are correlated to high tumour burden in seminoma and recurrence in NSGCT.


.png)
